The saying “An apple a day keeps the doctor away” is often used as a message of personal responsibility to our health. However, for many people in the U.S., especially Black Americans, Native Americans, and Latinos, health has far less to do with personal choice and much more to do with where people live, how much they earn, how they are systematically treated by institutions, and whether those institutions were designed to serve them in the first place. This blog explores how age, race, gender, and socioeconomic background intersect to shape who has proper access to care and who does not.
Health disparities aren’t random; they follow persistent patterns across race, gender, and age. Disparities in these communities are rooted in complex histories of colonization, slavery, and systemic inequality. In the U.S., Black Americans live shorter lives than White Americans, while Native Americans face some of the highest rates of chronic disease. These differences are not because of genes, as many people claim, but are due to the result of structural inequalities and policy decisions that have excluded entire communities from full access to health. For example, these factors can be as simple as how some hospitals, in predominantly Black neighborhoods, often have fewer resources and worse outcomes than those in wealthier, whiter suburbs. This isn’t simply a coincidence. It is the outcome of redlining, disinvestment, and racial segregation in healthcare. Importantly, this is not a uniquely American issue. Similar patterns can be seen globally. In Australia, recent research has shown that Aboriginal and Torres Strait Islander people experience poorer health outcomes and reduced access to care in regions where there is higher level opposition to Indigenous rights, directly related to the opposition of the Voice referendum, a proposed reform to give Indigenous people more political representation. Health isn’t just about what happens in a doctor’s office, it’s about the world people live in, starting even before birth.

From the very beginning of life, health is affected by these external conditions. Prenatal care, early childhood nutrition, and access to safe housing are all factors to having a foundation of long-term health. Yet many Indigenous and Latino children grow up in underfunded neighborhoods where they may attend schools without nurses or are even breathing air polluted by decades of industrial development. Take Cicero, a predominantly Latino community in Chicago. In 2023, air quality sensors revealed that Cicero’s pollution levels were significantly worse than other industrial corridors in Chicagoland. The poor air quality is due to the long history of heavy industry and lack of parks and trees, affecting and releasing harmful pollutants that include cancer-causing compounds, disproportionately affecting children. At the other end of life, elderly Black and Native American populations often struggle with adequate elder care. This is due to the long-standing mistrusts of medical institutions, rooted in centuries of abuse and neglect. In some cases, elders choose to avoid the healthcare system entirely. And when they do seek treatment, they are faced with providers who dismiss their symptoms or ignore their expertise, thus continuing this cycle of neglect.
Women of color face a distinct set of challenges, stemming from both racism and sexism. Black women, for example, are three times more likely to die from pregnancy-related causes than White women. This is due to how women of color are dismissed when they report pain and symptoms, leading to delays in diagnosis or even delays of treatment while in the hospital. Women of color are also less likely to be referred for specialty care, less likely to receive pain medication, and more likely to manage chronic conditions without adequate support. This affects how women of color navigate their daily lives; many may have to work in jobs that don’t offer health insurance or take on the caring role of sick family members without support. Public Health campaigns are also an issue, especially because they center White middle-class women while ignoring the realities of Black, Indigenous, and Latina women. This also includes a focus on trans and nonbinary people and their denial of care, harassment by providers and higher rates of mental health distress due to ongoing social exclusion. Immigration status also impacts the way in which individuals access or choose not to access healthcare for fear of deportation, discrimination, or language barriers.
While this blog focuses mostly on the U.S., turning briefly to Mexico offers an important lens for understanding how, in this specific case, Indigenous peoples’ experiences are shaped in different national, cultural, and political contexts. Making direct comparisons between countries is difficult, not only due to differences in data collection but also in the way indigeneity is defined. In Mexico, while education is often considered a key determinant of health, studies show it only partially explains Indigenous health disparities. Measures like income and employment, grounded in formal labor markets, don’t reflect the lived economic conditions of Indigenous peoples, many of whom engage in informal and traditional economies, or are not even considered to begin with. Still, important patterns emerge. For both the U.S. and Mexico, education is often seen as a key driver of better health. Yet, studies show that for Indigenous people in Mexico, higher educational attainment doesn’t always lead to improved health outcomes like it does for White populations. This shows that even when individuals “succeed” based on conventional markers like education, systemic barriers like racism and cultural misrecognition continue to shape healthcare in unequal ways.
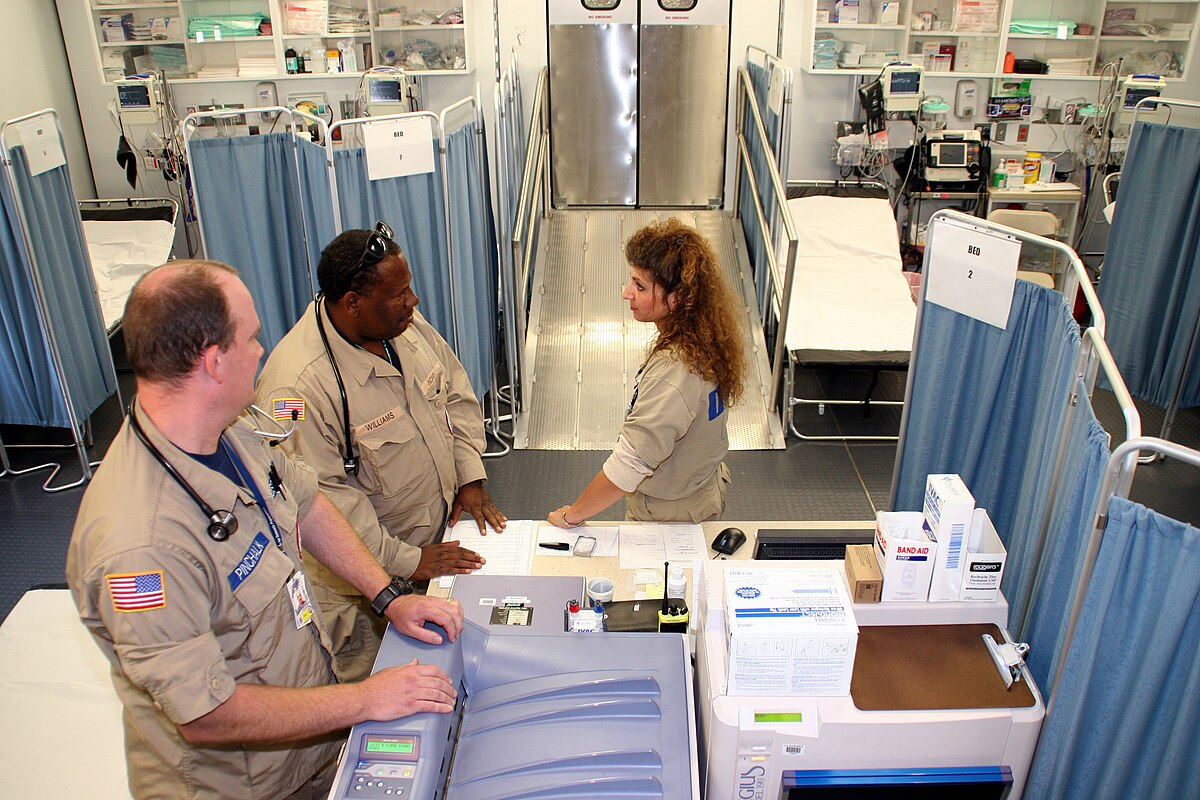
The most consistent theme, however, is the role of race in shaping access to health. Structural racism is a reality many people face daily. From segregated hospitals to discriminatory medical school curricula, the entire healthcare system has been built on racial inequities. Public health has been treated as a “field” separate from medicine, resulting in less funding, prestige, and institutional power. This division leaves women of color behind. While medical advancements get headlines, public health workers, many of whom are women of color, are left struggling to address basic needs like housing, food, and clean water. Black and brown women disproportionately provide unpaid or underpaid care for others, from nursing homes to hospitals to private homes. Yet, their own access is often limited. This poses the questions of who gets to be cared for in this society?
Solutions need to move from only being surface level. Diversity initiatives and cultural competency trainings aren’t enough. Real change means addressing the root causes of these issues of poverty, racism, environmental injustice and gender discrimination. Actively listening to communities, supporting local health workers, and making sure everyone has access to food, shelter, and clean air could be the beginning of this shift. One approach, called “community-centered care,” redefines health not as an individual achievement but as a collective responsibility by centering those on the frontline, women, elders, trans folk and immigrants. When looking at who gets sick, who gets treated, how they get treated, and who gets better, we are seeing a reflection of society. For Black Americans, Native Americans, and Latinos, health is a daily negation with a system that often excludes them. By working to eliminate systemic barriers to healthcare, expanding access to culturally competent care, and addressing the unique needs of these communities, we can take meaningful steps toward achieving healthcare equity for all.
Montiel is a guest blogger at UITAC Publishing. UITAC’s mission is to provide high-quality, affordable, and socially responsible online course materials.
Images used in this blog:
- FEMA – 18213 by Robert Kaufmann is licensed by Wikimedia Commons under the public domain. This image has not been altered.
- Cicero, IL by David Wilson is licensed by Wikimedia Commons under the Creative Commons Attribution 2.0 Generic license. This image has not been altered.