 Racial discrimination remains a deeply rooted issue in the United States, and its effects extend far beyond social and economic spheres, reaching into the very heart of the healthcare system — a system expected to serve everyone with an equitable level of care. Although this expectation exists, health disparities are far too common among racial minority groups, both in and outside of the United States. Researchers found that racism, in Europe, reinforces inequities in healthcare access and quality for racialized migrants. Researchers also found that various minority groups in South Africa face ethnic health disparities in the post-apartheid era. Despite advances in medical science within the United States, disparities in healthcare experiences, treatment, and health outcomes continue to negatively affect African American, Hispanic, and other marginalized communities at disproportionate rates.
Racial discrimination remains a deeply rooted issue in the United States, and its effects extend far beyond social and economic spheres, reaching into the very heart of the healthcare system — a system expected to serve everyone with an equitable level of care. Although this expectation exists, health disparities are far too common among racial minority groups, both in and outside of the United States. Researchers found that racism, in Europe, reinforces inequities in healthcare access and quality for racialized migrants. Researchers also found that various minority groups in South Africa face ethnic health disparities in the post-apartheid era. Despite advances in medical science within the United States, disparities in healthcare experiences, treatment, and health outcomes continue to negatively affect African American, Hispanic, and other marginalized communities at disproportionate rates.
For generations, minority communities have expressed distrust in the U.S. healthcare system due to experiences of discrimination and biased care. Researchers have found that experiences of discrimination in the healthcare system appear more common than previously recognized and deserve considerable attention. Researchers indicate that “[c]ompared with non-Hispanic White respondents, higher proportions of Hispanic respondents, non-Hispanic Black respondents, and non-Hispanic respondents with other racial/ethnic identities reported experiences of discrimination.” Nong and colleagues also found that 22.9 percent of Hispanic respondents, 22.8 percent of non-Hispanic Black respondents, and 23.4 percent of non-Hispanic respondents with other racial/ethnic identities reported experiences of racial discrimination compared to only 20.3 percent of non-Hispanic White respondents. Additionally, their five most commonly reported types of discrimination, race/ethnicity; educational or income level; weight; sex; and age, 17.2 percent of reported experiences of discrimination were based on race and/or ethnicity. They also found that 20.3 percent of individuals who experienced racial discrimination in healthcare settings experienced it four or more times.
Historical trends of unethical practices, within the U.S. healthcare system also contribute to the distrust of the healthcare system within minority communities. One example of unethical practices within the healthcare system is California’s eugenics practices. Although eugenics had been practiced worldwide, the purpose of eugenics within the U.S. was to inhibit specific communities from reproducing. While California’s sterilization program was officially dismantled in 1979, the state possessed a long history of sterilization dating back to the early twentieth century. The definition of eugenics is described as “good birth,” which suggests a suitable goal for all prospective parents, yet its historical connotations tie the practice to appalling policies, including forced sterilizations. often through surgical procedures like hysterectomies, tubal ligation, or vasectomies. Many of these practices were performed particularly on minority communities in state hospitals or correctional facilities. Researchers found that between 1920 and 1945, eugenic sterilization practices were disproportionately applied to Latinx patients, particularly Latina women and girls.

Another example of unethical medical practices within the U.S. is the Tuskegee Syphilis Study. In 1932, the small town of Tuskegee was one of the poorest towns in the U.S., and it was also primarily comprised of African Americans. The Tuskegee Study was conducted from 1932 to 1972 and involved researchers monitoring the progression of syphilis through 399 poor, African American males. Treatment, which became available just 11 years after the initiation of the study, was withheld from the participants for the duration of the study. An additional 201 non-syphilitic, poor, African American men were also unknowingly involved in the study as control subjects. During this study, researchers lied to both healthy and sick patients about their conditions, leading them to believe they were receiving treatments for “bad blood,” when in fact they were only receiving painful spinal taps to check for the presence of neural syphilis as part of the study. Ultimately, this resulted in some of the infected patients dying from the disease, when, in the case of later deaths, treatments were available that may have prevented this outcome.
As a result of the above–mentioned factors, as well as many other influencing factors, minority populations suffer disproportionately higher rates of negative health conditions, including chronic illnesses, preventable diseases, and untreated conditions. According to researchers, “[f]or racial and ethnic minorities in the United States, health disparities take on many forms, including higher rates of chronic disease and premature death compared to the rates among whites.” Obesity, a condition that has many associated chronic diseases and debilitating conditions, also largely affects minority communities. This has major implications for the quality of life and wellbeing for these population groups and their families. Research found that from 2011 to 2014, Hispanic children and adolescents ages 2 to 19 had the highest prevalence of obesity in the United States. Heart disease and cancer are the leading causes of death across race, ethnicity, and gender. Research also found that in 2010, African Americans were 30 percent more likely than Whites to die prematurely from heart disease and that nearly 44 percent of African American men and 48 percent of African American women possessed some form of cardiovascular disease. Additionally, researchers discovered that African American women were more likely to die from cancer compared to their White counterparts. Even the overall life expectancy has disproportionate negative effects on minority communities. Based on research conducted in 2016, the life expectancy of African American women, in 2012, was 78.4 years of age compared to 81.2 years of age for non-Hispanic White women. On the other hand, the life expectancy of African American men was 72.3 years of age compared to 76.5 years of age for non-Hispanic White men.
 The ongoing experiences of racial discrimination in the U.S. healthcare system, along with a long history of unethical medical practices and systemic neglect, reveal a deeply rooted pattern of injustice that continues to harm minority communities. From the history of unethical medical practices to the present-day disparities in patient diagnoses and treatment, communities of color have consistently faced barriers to equitable institutionalized racism, implicit bias, and a medical system that has too often devalued the lives and voices of African American, Hispanic, and other marginalized groups. As a result, these populations continue to suffer from worse health outcomes, higher rates of chronic illnesses, and lower life expectancy. The ongoing experiences of racial discrimination in the United States healthcare system, along with a long history of unethical medical practices and systemic neglect, reveal a deeply rooted pattern of injustice that continues to harm minority communities. From the history of unethical medical practices to the present-day disparities in patient diagnoses and treatment, communities of color have consistently faced barriers to equitable institutionalized racism, implicit bias, and a medical system that has too often devalued the lives and voices of African American, Hispanic, and other marginalized groups. As a result, these populations continue to suffer from worse health outcomes, higher rates of chronic illnesses, and lower life expectancy.
The ongoing experiences of racial discrimination in the U.S. healthcare system, along with a long history of unethical medical practices and systemic neglect, reveal a deeply rooted pattern of injustice that continues to harm minority communities. From the history of unethical medical practices to the present-day disparities in patient diagnoses and treatment, communities of color have consistently faced barriers to equitable institutionalized racism, implicit bias, and a medical system that has too often devalued the lives and voices of African American, Hispanic, and other marginalized groups. As a result, these populations continue to suffer from worse health outcomes, higher rates of chronic illnesses, and lower life expectancy. The ongoing experiences of racial discrimination in the United States healthcare system, along with a long history of unethical medical practices and systemic neglect, reveal a deeply rooted pattern of injustice that continues to harm minority communities. From the history of unethical medical practices to the present-day disparities in patient diagnoses and treatment, communities of color have consistently faced barriers to equitable institutionalized racism, implicit bias, and a medical system that has too often devalued the lives and voices of African American, Hispanic, and other marginalized groups. As a result, these populations continue to suffer from worse health outcomes, higher rates of chronic illnesses, and lower life expectancy.
Jackson is a guest blogger at UITAC Publishing. UITAC’s mission is to provide high-quality, affordable, and socially responsible online course materials.
Images Used in this Blog:
- “Racism in healthcare: Statistics and examples” by Mathieu Reese is licensed by Medical News Today. This image has not been altered.
- “Discrimination in the healthcare system is leading to vaccination hesitancy” by Gabriel Sanchez, Matt Barreto, Ray Block, Henry Fernandez, and Raymond Foxworth is licensed by Brookings. This image has not been altered.
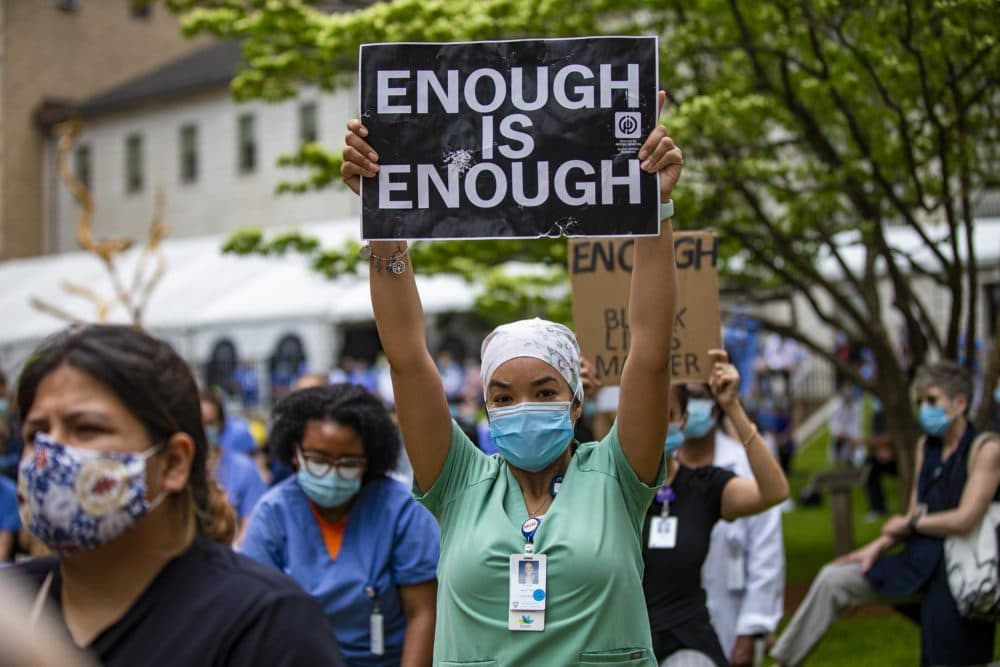
- “Racism In Medicine Isn’t An Abstract Notion. It’s Happening All Around Us, Every Day by Ayotomiwa Oja is licensed by WBUR. This image has not been altered.